by Ben Taylor
Precautions in place as Ebola outbreak spread in eastern DRC
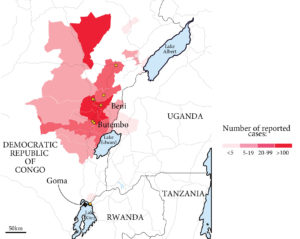
DRC affected health zones and ebola cases as of July 31, 2019; Uganda cases as of June 21, 2019 – Information from Reuters
Dr Faustine Ndugulile, the Deputy Minister of Health, Community Development, Gender, Elderly and Children, said the government has taken measures to install scanners in all entry points including airports and borders to prevent Ebola from entering the country.
More than 1,800 people have died and more than 2,700 have been infected in the latest outbreak of Ebola in central Africa, which began in August 2018. The World Health Organization (WHO) has declared the crisis a public health emergency of international concern.
The outbreak is the second-largest in the history of the virus. It follows the 2013-16 epidemic in West Africa that killed more than 11,300 people. It took 224 days for the number of cases to reach 1,000, but just a further 71 days to reach 2,000. About 12 new cases are being reported every day.
“The government has embarked on training to health personnel to provide them expertise on how to attend such patients,” said the Minister. “Surveillance systems have been set at the borders and airports. Motor vehicles from outside the country will be tracked, and isolation centres, laboratory systems and tourist monitoring systems have been put in place to ensure the country is ready for the fight against the disease,” he added.
The current 12-month epidemic began in the eastern region of Kivu in the DR Congo and cases have since been reported in neighbouring Ituri.
A case in late July in the border transport hub of Goma is of particular concern to authorities, as it is the first case in the city to be confirmed as transmission within the city. The two previous cases were patients who travelled to Goma after contracting the disease elsewhere. It is far harder to isolate patients and trace contacts in major cities, where large populations live in close proximity. Goma also adjoins the city of Gisenyi in Rwanda, and people travel between the two places every day.
Rwanda has stepped up border monitoring and has urged its citizens to avoid “unnecessary” travel to DR Congo, while some 2,600 health workers had also been vaccinated. Ugandan health officials are also screening travellers at the border to check their temperature and disinfect their hands, and some mass gatherings including market days and prayers have been cancelled. Three people died in Uganda in June, though the country has since been declared Ebola-free.
The WHO, however, stressed that no country should close its borders or place any restrictions on travel or trade, adding that the risk of the disease spreading outside the region was not high. WHO chief, Tedros Adhanom Ghebreyesus, said “we need to work together in solidarity with the DRC to end this outbreak and build a better health system.”
The fatality rate from Ebola is high – up to 90%, according to the WHO, and there is no proven cure as yet. However, rehydration with oral or intravenous fluids and the treatment of specific symptoms can improve survival – especially if the virus is caught early.
A multiple drug trial is currently under way in DR Congo to fully evaluate effectiveness, according to the WHO. An experimental vaccine, which proved highly protective in a major trial in Guinea in 2015, has now been given to more than 130,000 people in DR Congo, and thousands of health workers across the region have also been vaccinated.
(BBC, Al Jazeera, The Citizen)
Dengue fever outbreak
An outbreak of dengue fever, centred on Dar es Salaam, has caused widespread concerns and prompted a concerted government response.
“Dengue fever is here,” confirmed the Deputy Minister, Dr Faustine Ndugulile, in April. “We have started diagnosing some people, who suffered from the disease in Dar and Tanga regions. So I would like to advise health service providers to test patients, who, if diagnosed with the disease, should be provided with proper treatment,” he added.
By mid-May, the Ministry had confirmed 1,901 people had been diagnosed with the fever since it was first reported in January this year, 95% of whom are in Dar es Salaam.
Chief Medical Officer Prof Muhammad Kambi said the government has also increased surveillance in other regions, which have not been hit by the viral disease. He further said the government has ordered more test kits with capable of diagnosing 30,000 patients.
Dar es Salaam Regional Medical Officer Dr Yudas Ndungile said the regional authorities have taken various measures to fight the disease, citing destruction of mosquito breeding sites and public awareness about the disease particularly in the hardest-hit wards.
By July, the number of cases had dropped significantly, aided by end of the rainy season: 2,759 cases were recorded in May, which fell to 790 in June. Four cases were reported to have resulted in fatalities.
The disease is caused by Aedes Egypt mosquito that bites in daylight and harboured in stagnant water. (The Citizen)
Unsafe abortion: A silent killer of young women
Abortion in Tanzania is illegal. This makes it harder for girls and women to get access to safe abortion. Despite this, women still find their own ways to terminate unwanted pregnancies. Women use various methods including herbs and sharp instruments.
The problem of unsafe induced abortion is reflected in hospital statistics, which show significant numbers of alleged miscarriage. Given the legal restrictions associated with abortion, it is difficult to obtain reliable information on its prevalence and to assess the magnitude of the morbidity and mortality associated with it.
Nevertheless, according to the Ministry of Health and Social Welfare, 16 percent of maternal deaths are due to complications from abortion.
Further, in a nationally representative study of the incidence of abortion and the provision of post-abortion care in Tanzania, researchers found that clandestine abortion is common and is a major contributor to maternal death and injury. Tanzania’s national abortion rate—36 per 1,000 women of reproductive age—is similar to that in other East African countries.
The Penal code provisions on termination of pregnancy are frequently misunderstood as a total prohibition on abortion. Under section 230, it is stated that termination of pregnancy is lawful where it is done to preserve the life or health of the pregnant woman. Nevertheless, any person who assists in an illegal abortion breaks the law, including the pregnant woman herself, anyone who assists her to procure an illegal abortion, and the supplier who provides drugs or equipment used to induce an illegal abortion.



